In the care and treatment of the heart, a nihilistic approach, do not touch, let alone plan, and
perform an operation was founded in the lack of any chance of helping heart patients over the
millennia. Starting slowly with looking at the anatomic defects upon death of a heart patient in the mid
1600’s and gaining momentum with shunt procedures. The most notable shunt procedure emerging
from the research labs to successful surgeries for some of the blue babies in 1944 was the Blalock-
Taussig-Thomas shunt. The surgical shunt procedures, did not require entering the heart’s four
chambers, and they helped the doomed blue babies. As World War II was ending, these shunt
procedures also accelerated the desire for a heart lung machine.
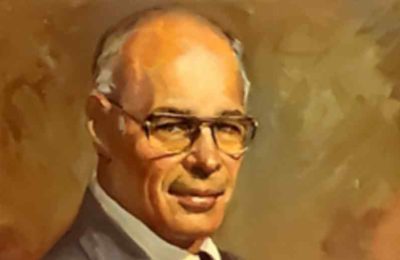
In Spokane, the heart teams picked up this momentum when Dr. Ralph Berg moved to Spokane,
Washington, his home town, in January 1952. He was well trained in chest surgery, as his chest
fellowship was taken with Dr. Evarts Graham, the father of chest surgery. Berg was also keenly focused
on the care of blue babies and the associated pursuit of a heart lung machine. It was conceptualized that
such a machine would allow more time inside a heart, to perform a more complicated repair.
Once settled in Spokane, Dr. Ralph Berg set up a research lab and continued to research each
advance during the pursuit of the heart lung machine. Engaged in fund raising, community education as
well as his chest surgery practice, Dr. Berg was using hypothermia and swift surgical technique to
perform closures of single defects between the heart chambers, considered an intracardiac repair.
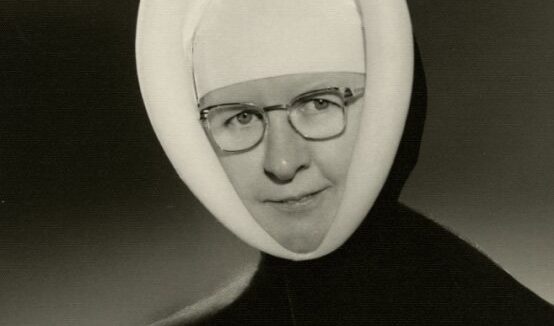
Then a most fortuitous and amazing thing happened. Sister Mary Bede was scheduled to come to
Spokane to administer and support Sacred Heart Hospital. Before she arrived, she visited and met Dr.
Berg. She then moved forward and supported the research lab, providing both an upgrade and
expansion of the lab and purchased a heart lung machine. Her goal in 1955 was to make every mistake
in the research lab, then take the machine to patients.
With the new lab, essentially an operating room of equal quality, yet for smaller patient’s, i.e. a dog, and
one of the first commercially available heart lung machines, the Spokane team was poised to delve into
the heart lung machine pursuit. The heart team also grew with the addition of a pediatric cardiologist
and a vascular surgeon. Both physicians were attracted to the pursuit of a heart lung machine as well as
to heart surgeon Dr. Ralph Berg. The team began its experiments and quickly learned the oxygenator
needed to be upgraded.
During this time, fund raising and community education continued. The team learned and dealt with
multiple problems in addition to the oxygenator. The overarching issue was Dr. Ralph Berg could
perform the same procedures on his young human patients successfully with his swift surgical technique
and hypothermia. He was therefore not interested in moving forward with the heart lung machine until
those results were at least close to his hypothermia case results. A total of three oxygenator upgrades,
about fifty research labs were performed before this team was ready to go live with the transition to a
young female who was crippled by her blue baby defect.
And so, when the first case was done in January of 1959 with such success it was anticlimactic, the team
was set to take on all aspects of the heart. Spokane, a mid-sized community, without an academic
institution and without a federal grant was several years ahead. The team did not publish the first series of patients. The mortality was two percent and the team felt this was acceptable. However, across the
country and the globe the mortality for on pump, heart lung machine cases the mortality was still much
higher.
This team stayed together. The vascular surgeon dropped off the team by 1963 as he did not need this
technology for his patients. The pediatric cardiologist worked diligently with Dr. Ralph Berg and even
converted to an adult cardiologist when the number of blue babies dwindled and the number of adult
heart patients began to explode by 1967. When Dr. Francis Everhart came to Spokane in 1968, to work
with this team all the pieces were in place to support the voluntary, two-tiered protocol that developed
and launched in June of 1970. The work done during the pivotal decade is called the Spokane
Experience.